The COVID-19 pandemic has significantly impacted global healthcare systems, with patient outcomes varying widely from asymptomatic cases to severe illnesses, resulting in high mortality. Understanding which factors contribute to poor prognosis is crucial in managing the disease effectively. Chest imaging has been pivotal in diagnosing and assessing the severity of COVID-19, with computed tomography (CT) scans revealing characteristic pulmonary changes. Recent research has turned to extrapulmonary manifestations, such as pleural effusion (PE), and their potential role as prognostic markers. A German multicentre study explored this concept, focusing on the prevalence of PE in COVID-19 patients and its association with clinical outcomes like 30-day mortality, intensive care unit (ICU) admissions, and mechanical ventilation requirements.
Prevalence of Pleural Effusion in COVID-19 Patients
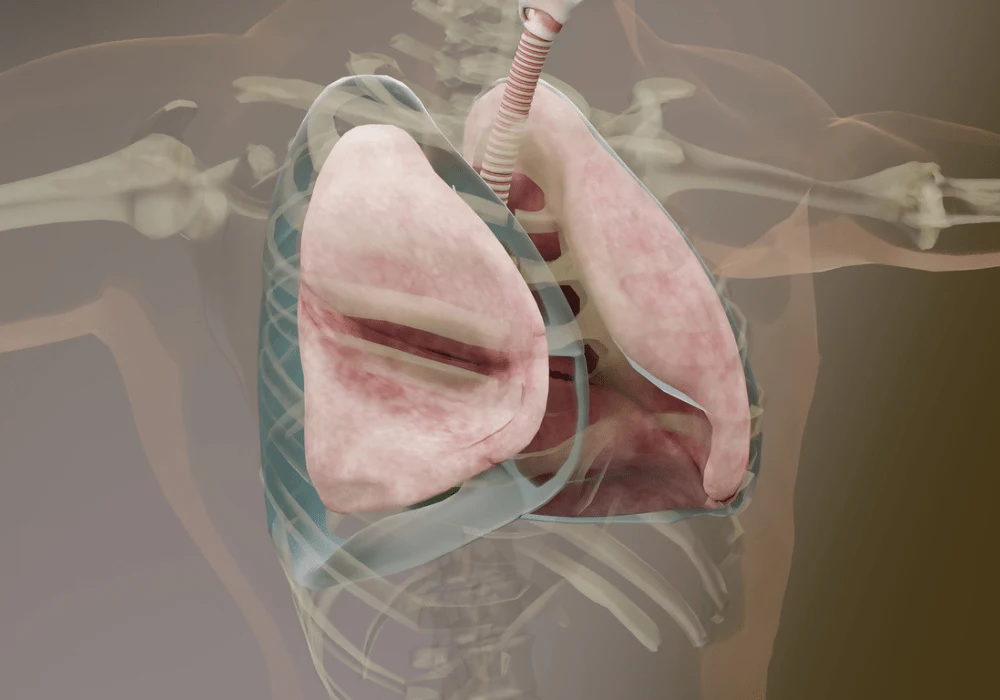
The study examined 1,183 patients across multiple centres in Germany, finding that pleural effusion was present in about 31.5% of patients. PE, which is an accumulation of fluid in the pleural cavity, was once considered an uncommon manifestation of COVID-19 but is now recognised as more prevalent than initially thought, especially among critically ill patients. Its development in COVID-19 can be attributed to factors such as severe lung inflammation, viral pleuritis, secondary bacterial infections, or systemic responses leading to conditions like heart failure.
While the study did not find a significant association between the volume or density of PE and mortality, the presence of PE alone was found to be a notable predictor of 30-day mortality. PE occurred in 47.5% of non-survivors compared to 27.3% of survivors, and patients with PE had a 2.22 times higher hazard ratio for 30-day mortality. This suggests that detecting PE early in COVID-19 patients can provide valuable prognostic information.
Association with Clinical Outcomes: Mortality, ICU Admissions, and Ventilation Needs
The study's findings indicate that the presence of PE is not only associated with increased mortality but is also correlated with the need for ICU admission and mechanical ventilation. Among the patients, 46.8% required ICU care, and 26.7% required mechanical ventilation, with PE being a significant factor in these outcomes. The multivariable regression analyses showed that the presence of PE predicted ICU admission and the need for ventilation independently, underscoring its role as a critical factor in clinical decision-making.
Interestingly, while PE volume and density were not linked to patient outcomes, a higher COVID-19 CT score, reflecting the extent of lung damage, was associated with all the investigated clinical outcomes. This highlights that the presence of PE and the extent of lung damage are independent but complementary factors in assessing the prognosis of COVID-19 patients. These findings emphasise that radiological reports should prioritise the identification of PE, as it has actionable prognostic value without the need for detailed measurements of its volume or density.
Gender-Specific Findings and Clinical Implications
The study also observed differences in the prevalence of PE between male and female patients, with a higher prevalence in females (39.4%) compared to males (28.2%). However, no significant differences were found in the volume or density of PE between genders. The predictive association of PE with mortality, ICU admission, and the need for mechanical ventilation remained consistent across genders, indicating that the presence of PE is a significant prognostic marker regardless of gender.
These findings have substantial implications for the clinical management of COVID-19. By identifying PE as a straightforward and independent prognostic indicator, clinicians can better stratify patients based on their risk of severe outcomes. This can help in triaging patients who may require closer monitoring, early ICU admission, or prompt intervention to mitigate worsening respiratory conditions. Early PE detection by using CT imaging allows for a more personalised and effective treatment, potentially improving patient outcomes.
The German multicentre study highlights the prognostic significance of pleural effusion in COVID-19 patients. The presence of PE independently predicts increased 30-day mortality, ICU admission, and the need for mechanical ventilation, making it a valuable factor in assessing the severity of the disease. Since the volume or density of PE does not significantly impact outcomes, identifying its presence should be prioritised in radiological evaluations of COVID-19. This study contributes to the growing body of evidence supporting the use of CT imaging for diagnosis and prognostication in COVID-19, ultimately aiding clinicians in risk stratification and personalised patient management.
Source Credit: Cardiothoracic Imaging
Image Credit: iStock
References:
Buchera A M, Henzela K, Meyerb H J et al. (2024) The prognostic relevance of pleural effusion in patients with COVID-19 - A German multicenter study. Cardiothoracic Imaging. 110303