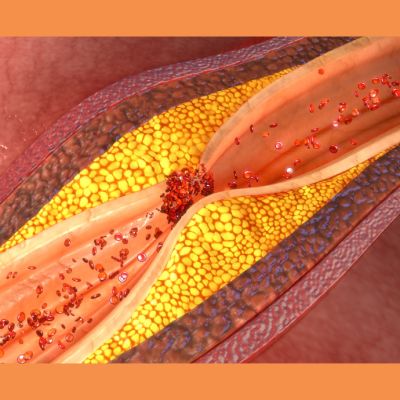
In patients with chronic obstructive pulmonary disease (COPD), symptoms like dyspnea, wheezing, and coughing are common and indicate a faster disease progression and higher mortality. These symptoms can be caused by various factors, including muscle weakness, airway obstruction, chronic inflammation, and structural changes in the airways. Studies have shown that airflow turbulence and particle deposition increase with surface roughness of the trachea, and histopathological evidence suggests similar inflammation and remodelling occur in both central and peripheral airways. However, current methods for assessing tracheal abnormalities are limited in their ability to capture the overall surface morphology. A recent study published in Radiology Advances aims to develop a new approach using fractal analysis to quantify tracheal surface roughness in COPD patients, expecting it to be higher in COPD individuals and associated with airflow limitation and worsened symptoms like dyspnea, wheezing, and cough.
Study Overview and Participant Demographics
The study drew participants aged over 40 from the Canadian Cohort of Obstructive Lung Disease (CanCOLD), a multicenter population-based study conducted between 2009 and 2015. Ethical approval was obtained from each participating institution, and written informed consent was provided by all participants. COPD status was determined based on a forced expiration volume in 1 second/forced vital capacity (FEV1/FVC) ratio of less than 0.70. Participants were categorised into four groups: never smokers without COPD, ever smokers without COPD, mild COPD (Global Initiative for Chronic Obstructive Lung Disease [GOLD] stage I), and moderate to severe COPD (GOLD stage II or higher). Follow-up visits were scheduled every 18 months for data collection. Among the initially recruited 1561 participants, 308 were excluded due to missing data on CT imaging, spirometry, plethysmography measurements, or smoking history, resulting in a final sample size of 1253 participants. Pulmonary function tests, including spirometry (FEV1, FVC, and forced expiratory flow between 25% and 75% of FVC [FEF25–75%]), and total lung capacity (TLC) measurements using whole-body plethysmography, were conducted. Health status was assessed using the COPD assessment test (CAT), with a CAT score of 10 or higher indicating a significant health impact. Dyspnea was evaluated using the Medical Research Council (MRC) dyspnea scale, with a score of 3 or higher considered clinically significant. Additionally, a lower cutoff of MRC score 2 was used to reflect the mildness of the CanCOLD cohort. Recurrent wheezes and persistent cough were recorded as binary data. Demographic and test results were analyzed across the different participant groups. Ever smokers without COPD had a slightly higher body mass index (BMI) compared to those with mild COPD. The mild COPD group had fewer females compared to both never smokers without COPD and moderate to severe COPD groups. Participants with moderate to severe COPD had a higher smoking history in terms of pack-years compared to ever smokers without COPD and those with mild COPD. Additionally, there were fewer ex-smokers in both mild and moderate to severe COPD groups compared to ever smokers without COPD, and the moderate to severe COPD group had more current smokers compared to both never smokers without COPD and those with mild COPD.
Association Between Tracheal Surface Roughness and COPD Symptoms
In a population-based study primarily involving individuals with mild COPD, researchers found that the roughness of the trachea lumen surface (SRS) was higher in participants with COPD compared to those without COPD. This increased roughness was associated with poorer lung function and a higher burden of COPD symptoms, regardless of other measures such as trachea index (TI) and whole-lung CT emphysema and airway disease measurements. Previous studies mainly used CT TI measurements to assess trachea abnormalities, but results were inconsistent. This study's novel approach of using SRS was more effective in quantifying differences in trachea surface abnormalities between COPD and non-COPD groups, especially in a mild COPD cohort. The SRS measurement was independently associated with COPD symptoms, such as dyspnea, even when accounting for other factors like TI and whole-lung measurements. This highlights the importance of considering tracheal surface topology, not just diameter, in understanding COPD severity and symptoms.
Significance of Tracheal Surface Shape in Airflow Dynamics
Furthermore, trachea surface shape abnormalities were shown to differentiate between participants with and without COPD and were linked to worse lung function and symptoms, independent of trachea curvature. This suggests that trachea surface shape plays a significant role in airflow dynamics. Various factors may contribute to trachea abnormalities in COPD, including airway inflammation, lung hyperinflation, and excessive coughing. Importantly, trachea abnormalities remained significant even after adjusting for emphysema, suggesting an independent association with lung function and symptoms in COPD. However, the study had limitations, such as only analysing inspiratory images and not investigating abnormalities requiring both inspiratory and expiratory scans. Future research should explore the clinical relevance of trachea analysis, establish normative values, and assess its role in predicting disease progression and guiding treatment decisions.
Quantifying trachea abnormalities using SRS measurement provides valuable insights into airflow limitation and symptom burden in COPD, offering a potential new biomarker for understanding and managing the disease.
Source: Radiology Advances
Image Credit: iStock